Supportive Services & Care Management
Our in-home and community-based services are available to all who meet the eligibility criteria without regard to race, ancestry, national origin, language, religion, gender identity or sexual orientation.
Creating a Community where all can age with Dignity and Independence
Home Care Program
The Home Care Program provides eligible individuals with the supportive services that they may need to live safely and independently at home.
What is the Home Care Program?
The Home Care Program provides eligible elders with the supportive services that they may need to live safely and independently at home. Services may include meal preparation, shopping, homemaking, personal care, emergency response systems, or adult day care.
How do I qualify?
A professional care manager from Elder Services will make a home visit to see if you are eligible for services. While there, the care manager will assess your health and social needs. You must be a resident of Massachusetts, be sixty years of age or older, and have a “critical need” for services. In addition, you must meet certain income guidelines.
During the home visit the care manager will determine your eligibility and work with you to develop a care plan that best meets your needs.
How do I make a referral for the Home Care Program?
You can make a referral through our Information and Referral Department. Call 508-595-8106 or use the on-line referral form on this website.
Who provides the Home Care services?
Elder Services has contracts with qualified provider agencies who perform the work or provide the service. Elder Services pays for the services with funds provided by the state. Your care manager will select the best provider in your neighborhood to perform the service for you, and work with you to ensure that your needs are being met.
Is there a cost for these services?
There may be a monthly charge for your services. The co-payment is based on your income, not your assets. The lower your income is, the smaller your payment will be. Elders with very low incomes are not charged any co-payment, but may make a donation.

Senior Nutrition Programs
Elder Services of Cape Cod and the Islands offers both Senior Dining Centers and Meals-on-Wheels. These programs are for individuals of all income levels age 60 and older.

Long Term Care Screening
Our Health Services Unit provides required screening for individuals seeking Medicaid reimbursed services such as nursing home care, adult day health programs or other community-based services.
Selecting Long-Term Care
Deciding whether to seek placement and then selecting a long-term care facility (nursing or rest home) can be a difficult and emotional process. The move to a long-term care facility is rarely anyone’s first choice. By being prepared, individuals can have more control over their lives and the transition can be smoother.
Long-Term Care Facilities
Nursing homes provide long-term skilled health care for residents whose needs cannot be met in the community. They are designed to care for people who are chronically ill or recuperating from an illness and need skilled nursing care, but do not require hospitalization. Rest homes provide custodial care for those who require room and board, supervision of personal care, and medication management, but do not require routine nursing services. Both nursing and rest homes are licensed and inspected by the state Department of Public Health.
Eligibility
Once the decision has been made to seek nursing home placement, medical eligibility must be determined through a long-term care “screening”. This screening is required for all individuals applying for Medicaid. It is also available, for a fee, to individuals who will be paying for their nursing home care with private funds.
The screening team will need to obtain information from the individual’s primary health care provider, so it is important for anyone considering a move to a nursing home to inform their physician and/or nurse of the decision to seek placement.
Contact the Elder Services Information and Referral Department to arrange for a screening at 508-394-4630 or 1-800-244-4630.
Paying for Long-Term Care
Rest home costs are covered by an individual’s ability to pay privately or qualify for social security disability insurance, or other benefits. While a rest home resident may use Medicare or Medicaid to pay for medical care, neither Medicare nor Medicaid will pay for room and board.
In nursing homes, costs may vary according to the level of care required and the extent to which it is covered by private insurance, Medicare, or Medicaid. It is important to realize that neither private nor public insurance cover all nursing home costs.
If the cost of care exceeds an individual’s income and assets, then the MassHealth Enrollment Center should be contacted for a MassHealth application. Call them at 1-800-242-1340.
If help is needed in determining financial eligibility, a consultation with an elder law attorney is recommended. SHINE counselors (Serving the Health Information Needs of Elders) also can assist with completing a Medicaid application. They can be reached at 1-800-334-9999.
Selecting a Facility
The goal should be to select the right facility for the individual, one which best meets his/her needs and assures safety and well being. Know what to look for and evaluate options.
Call the Admission Coordinators of the facilities being considered and arrange for a visit. Act like a consumer who is purchasing something of value. Visit more than one home and visit at different times of the day. During your visit, observe your surroundings. Note how residents are being treated by staff. Bring questions with you and inquire about facility policies for issues such as personal possessions, room assignments and changes, and visiting hours. Give an accurate description of the individual’s physical status and care needs to the Admission Coordinator to be sure that the facility can provide the necessary care.
Residents’ Rights
All nursing and rest home residents are protected by federal and state laws and have specific rights regarding their treatment and care. Elder Services’ Long Term Care Ombudsman Program can assist in the protection of residents’ rights. Ombudsmen visit facilities on a weekly basis to monitor conditions and to address residents’ complaints. The Ombudsman Program is also a good resource for information about the selection and admission process and other nursing/rest home related issues.
How to Get Good Care
Once a nursing/rest home has been selected and the new resident has settled into the facility, many family members are uncertain about their continuing responsibilities. They may feel that since they are no longer assisting with activities such as personal care, help at mealtime, or transportation to medical appointments then their role as a caregiver is over. Actually, the family member is just entering a new phase of care-giving by assuming the role of an advocate for good care.
An effective advocate:
- Becomes educated about resident rights
- Stays involved and visits often
- Observes conditions and asks questions
- Learns the names and positions of key staff
- Develops mediation/negotiation skills
- Avoids confrontational behavior
- Helps the facility to see the family member as part of the care-giving team
One good way to make sure that a resident is receiving good care is to regularly attend care-planning meetings.
Every new resident receives a comprehensive evaluation by the various departments of the facility (physical therapy, nursing, dietary, activities) and the collected information becomes part of the resident’s care plan. This plan is reassessed at least once every ninety days. The resident and family members can be present at these meetings and they provide an excellent opportunity to ask key questions and to make sure that the different caregivers are functioning as a team.
The Ombudsman for the facility may attend as well to act as an advocate for the resident.

Options Counseling
Options Counseling is short-term decision support counseling to help you in making an informed choice about your long-term services, supports and settings. It is available to adults age 60+ or living with a disability regardless of income.
What is Options Counseling?
Options Counseling is an interactive, short-term decision-support process to assist consumers of any income (elders age 60 or over, or individuals over the age of 18 with any disability) and their family members, caregivers and/or significant others to make an informed choice about long term services, supports, and setting.
Primary Consumers Seen by Options Counselors:
Consumers in hospitals and rehabilitation facilities, at risk of discharge to a long term care facility.
Consumers in a long term care facility seeking to return to a community setting.
Settings where counseling service is provided include:
- Hospitals
- Nursing Facilities
- Rehabilitation Facilities
- Community Settings
- Home Settings
Methods of delivering services:
- Telephone
- Face-to-face
- Via e-mail
- Service Provided to Consumer:
The Options Counselor first looks to identify the goal of the consumer: to transition out of the nursing home back into the community, to remain in the community with services or to seek nursing home placement. The Options Counselor then provides:
- Unbiased information about long term services and supports;
- Information about resources available to pay for the services;
- A consumer-driven approach that ensures the consumer’s personal goals and preferences are respected;
- Options Counseling provided in a timely and appropriate manner based on the consumer’s situation;
- Identification of next steps;
- Assistance in facilitating referrals and resources as needed
Thirty days after the final counseling session, the Options Counselor contacts the consumer to determine whether the intended goal was met and to identify barriers if it was not. At that time the consumer will be asked to participate in a consumer experience survey via telephone, mail, or web based.
For more information or to make a referral, contact us at:
Elder Services of Cape Cod & the Islands
(508)394-4630, 1-800-244-4630
(508)394-8691(TTY)
www.escci.org
CORD
(508) 775-8300(V/TTY), 1-800-541-0282(V/TTY)
www.cilcapecod.org
cordinfo@cilcapecod.org

Family Caregiver Support Program
Strives to support and promote the ability of caregivers to continue in their caregiving role by helping them to make informed decisions, solve problems, and reduce stress.
The Family Caregiver Support Program advocates for caregivers. It provides the education, advocacy, and connections to the community resources that enable caregivers to better care for their loved ones as well as themselves. In-home and telephone assessments help to determine the caregiver’s needs and the appropriate services to be recommended. It facilitates connections to resources and education for caregivers of older adults, grandparents raising grandchildren, and older adults caring for individuals living with a disability.
While caregiving is universal, each caregiver comes to us with individual needs that may require only a brief connection, or a more in-depth service. Our support is delivered either over the phone or by an in-home or office visit, depending on the preference of the caregiver.
Who is Eligible?
- Caregivers age 60 and older
- Caregivers for adults age 60 and older
- Grandparents age 55 and older raising their grandchildren (under age 18)
- For those age 55 and older who care for a disabled individual who is not their child.
- Anyone caring for someone with Alzheimer’s Disease/dementia.
How do I make a referral for the Family Caregiver Support Program?
You can make a referral through our Information and Referral Department. Call 1-800-244-4630 or 508-394-4630 M-F 9AM to 5PM and ask to speak with an Information Specialist or use the on-line referral form on this website.
Services
- In-home, office or telephone assessment of caregiver needs
- Counseling related to caregiving concerns
- On-going support and family meeting facilitation
- Help with developing emergency, short-term and long-term plans
- Advocacy for caregivers and their families
- Connecting to community supports and resources
- Education, training and support
- Referrals to Caregiver Support Groups
Money Management Program
The Massachusetts Money Manager Program assists income-eligible adults aged sixty or older who may be at risk of losing their independence due to their failure to pay rent, utility or other basis bills on time.
The Massachusetts Money Management Program assists income-eligible adults aged sixty and older, who may be at risk of losing their independence due to failure to pay rent, utility, or other basic bills on time. Individuals request money management assistance for a variety of reasons including limited support, visual impairment, disability, or cognitive issues. This program is offered free of charge to income-eligible individuals and at a small fee to others.
Trained volunteer bill payers meet with individuals in their homes to help them pay monthly bills and manage their money wisely. Volunteers also help elders avoid becoming victims of fraud, scams, or financial exploitation.
The Massachusetts Money Management Program serving Cape Cod and the Islands was developed by Elder Services of Cape Cod and the Islands, Inc. in 1999. The Money Management Program is collaboratively sponsored by the Executive Office of Aging & Independence and Mass Aging Access.
Under the Massachusetts Money Management Program’s guidelines, volunteer bill payers assist individuals with budgeting, writing checks, balancing checkbooks, and reconciling bank statements. The individual makes all bill paying and budgeting decisions, remains in control of their money, and retains check-signing authority.
Money Management Volunteers are trained, insured, and supervised by the Program Manager. Program safeguards include monitoring and supervision of all volunteer activities, file monitoring, and an annual survey of all individuals served to assess satisfaction with the services provided.

Congregate Housing at Hansen Village
Congregate housing offers affordable and supportive shared living arrangements for adults over 60 or living with a disability as an alternative to premature nursing or rest home placement.
Congregate housing offers affordable and supportive shared living arrangements for adults over 60 or living with a disability as an alternative to premature nursing or rest home placement.
Our congregate house is located at the Hansen Village housing complex, a mixed use development operated by the Sandwich Housing Authority in conjunction with the Executive Office of Aging & Independence.
The residents of the Congregate House receive the supportive, social, and health services needed to assist individuals who want to continue living independently.
Residents maintain their own living units, but share common areas such as living rooms, dining, and kitchen facilities. An on-site coordinator helps to arrange needed services. To be eligible, an adult must qualify for public housing and be physically able to live on their own. Space is provided for residents to store their own food and prepare their own meals; an optional meal plan is available for the evening meal.
Congregate housing is appropriate for individuals likely to remain in the program for a minimum of one year barring infrequent and unexpected periods of acute illness.
To learn more about the Hansen Village Congregate House, contact the site coordinator at 1-508-888-1666.

Senior Care Options (Managed Care for MassHealth Enrollees)
The Senior Care Options (SCO) program is a Mass Health Program that covers all services reimbursable under Medicare and MassHealth through a senior care organization and its network of providers. The goal of the Senior Care Options programs is to help their consumers remain in the community as independently as possible.
Through the Senior Care Options program, a plan with $0 out-of-pocket costs, members receive a wide range of benefits and services, including dental care and transportation, coordinated by a primary care team. Members get services from their plan’s network of medical and other professionals, including a primary care doctor, nurses, specialists, and a Geriatric Social Support Coordinator from ESCCI.
SCO Eligibility Criteria:
- Age 65 or older
- MassHealth Standard
- If a Medicare beneficiary must have Parts A & B
- Primary Care Physician (PCP) and specialists in the SCO network
- For ESCCI, only Barnstable County residents are eligible (does not cover MV or Nantucket)
- There are no premiums or deductibles to join the SCO plan.
Enrollment in SCO is through the plan provider. ESCCI works with the following plans:
- Boston Medical Center Health Plan (855-833-8124)
- Fallon Community Health Plan (877-255-7108)
- Tufts Health Plan (855-670-5934)
One Care
One Care is a MassHealth Program that bridges the gap between your MassHealth benefits and Medicare benefits. With One Care, each member is provided with a Care Team that assists in coordinating each member’s care plan. Members get services from their plan’s network of medical and other professionals, including a primary care doctor, nurses, specialists, and a long-term support services coordinator from ESCCI.
One Care Eligibility Criteria:
- Must be between the ages of 21 and 64.
- Eligible for MassHealth Standard and Medicare.
- Live in the service area of the One Care plan.
- Agree to receive covered health care services exclusively through the One Care plan.
- PCP and any specialists seen must be part of the One Care network.
Enrollment in One Care is voluntary.
There are no premiums or deductibles to join the plan provided the member has MassHealth Standard. Click Here to learn more about One-Care
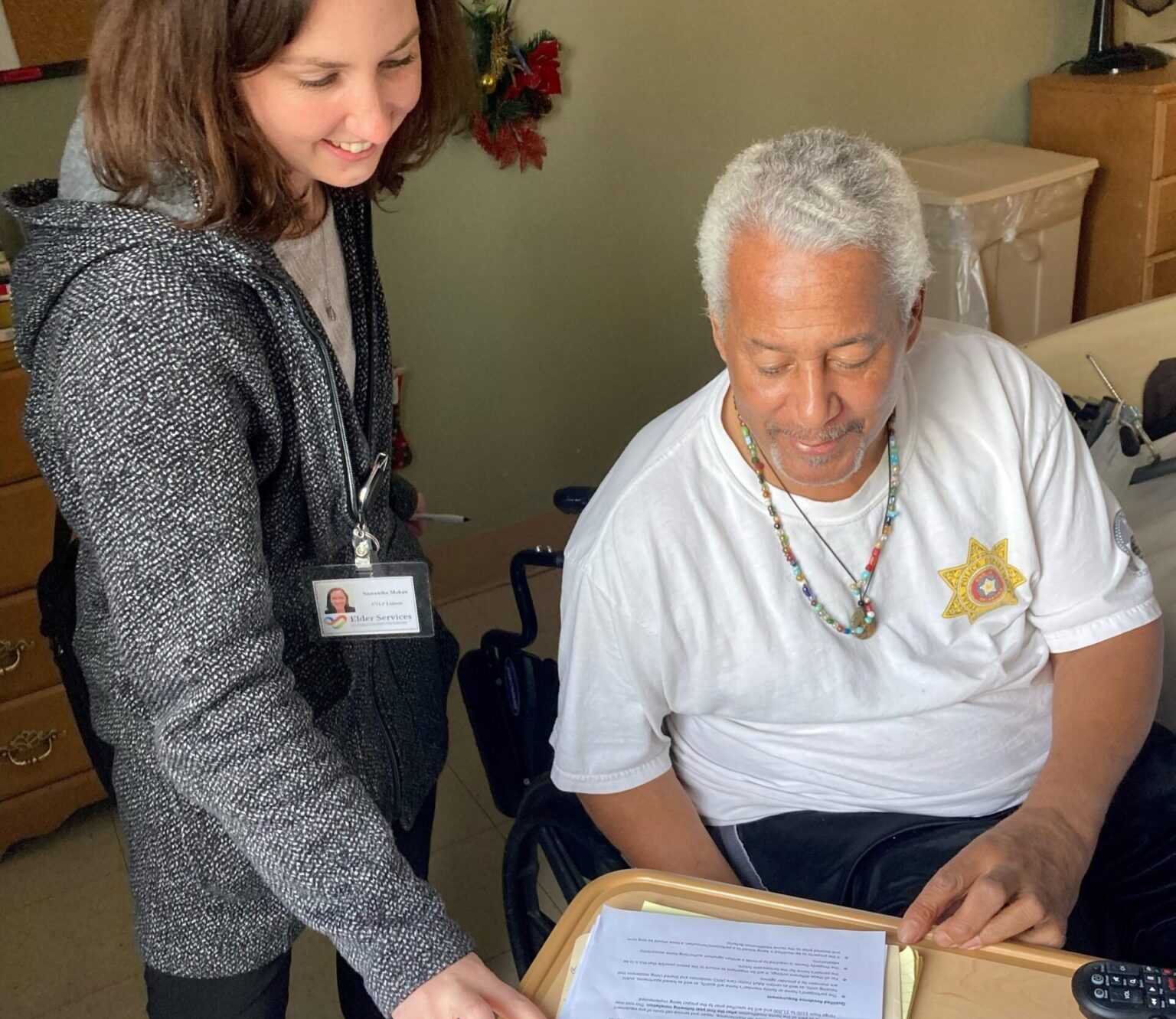
Community Transition Liaison Program
The Community Transition Liaison Program supports nursing facility residents age 22 or older in transitioning to the community.
The Community Transition Liaison Program (CTLP) assists nursing facility residents with any diagnosis or any type of insurance. The CTLP team supports any adult resident of a nursing facility who is interested in receiving support & assistance to transition to the community.
The CTLP team can assist nursing facility residents by:
• Meeting with residents to discuss their needs and providing options for a safe plan to return to community living;
• Assisting in identifying needs that should be addressed in discharge planning;
• Assisting with applications for housing and public benefits, including collecting all necessary documentation;
• Mitigating issues that may impact a resident’s ability to successfully transfer to the community;
• Coordinating with state and community agencies to identify resources and make referrals; and
• Providing other supportive services as appropriate.
The CTLP Team members visit area nursing facilities on a weekly basis and can be approached at that time. They can also be reached by calling our Information and Referral Department at 508-595-8106.